The first patients are expected to benefit from the new improved images in 2018.
The project revolves around infrared light and finding the ideal wavelengths. Optical crystal fibres and laser technology. And shrinking a laser source that roughly fills two offices into shoebox-sized device.
It draws on extensive knowledge of physics, optics, and advanced laser technology, combined with deep clinical knowledge of skin cancer and imaging, and applies this to help skin cancer patients get a faster diagnosis and the right treatment.
It aims to create ultra-high-quality skin images at rapid speed.
“When we use images for diagnosing skin cancer, it’s important that they are high quality, so that we can see many details beneath the skin’s surface. We want to be able to see the clear boundaries between the skin layers, and between the cancer and normal skin. When we have high quality images, we can quickly determine whether the patient has skin cancer. We can also see how much the cancer has spread in the skin—both in depth and in width. This avoids the need for the patient to have a tissue sample taken and wait several days for the test results. They can begin the right treatment more quickly,” says Consultant Mette Mogensen, PhD, Clinical Associate Professor, Dermatology Ward, Bispebjerg Hospital.
A painless investigation
Mette Mogensen has over ten years’ experience with skin cancer imaging and has been working with DTU Fotonik for just as long on technology that makes it possible to ‘look into’ the skin. The technology is called Optical Coherence Tomography (OCT), and first showed its potential for diagnostic imaging in the early 1990s.
OCT uses infrared light to see a few millimetres into the skin. The OCT method provides a real-time image of the tissue, while also being painless and non-invasive (no cutting or pricking).
In the Shape OCT project, researchers from DTU, Bispebjerg Hospital and elsewhere have teamed up to get OCT technology to deliver higher quality images. Being able to ‘look deeper’ into the skin is another key goal notes Professor Ole Bang from DTU Fotonik regarding the project, which has been running for three years.
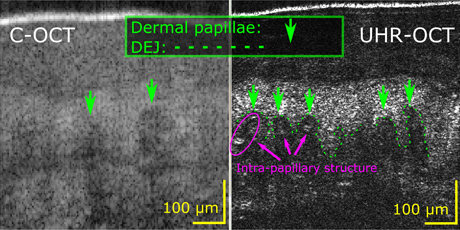
The left image shows the top layer of a healthy patient’s skin using conventional OCT equipment. The right image was made using DTU Fotonik’s improved OCT equipment, which shows more details. The extra detail is important when diagnosing skin cancer. Photo: DTU Fotonik
Challenges with depth
“We have successfully improved the OCT technology so it delivers more detailed images than the OCT devices on the market today. We are currently working on penetrating deeper into the skin using the infrared light, so we can create images that show how deep the cancer has progressed,” says Professor Bang.
"The great majority of our skin cancer patients will benefit from the faster new imaging, because their diagnosis will be made quickly following a painless examination, with the results available on the same day"
Mette Mogensen, Bispebjerg Hospital
Depth is something which is important to the examining doctors:
“It’s very important that we can see how deep the cancer has progressed, because this determines what treatment the patient should have—surgery, radiotherapy, or simply medication applied directly to the skin,” says Consultant Mette Mogensen.
But penetrating deeper into the skin is easier said than done. The laser source Ole Bang and his research team are working on is a ‘supercontinuum’ laser.
Most of us are familiar with laser beams as a powerful monochrome light beam. A supercontinuum laser makes it possible—by passing the laser beam through optical crystal fibres—to convert the powerful monochrome laser light into white light containing all the colours. This is because spectral dispersion of the light occurs inside the crystal fibre (the light goes from one wavelength/colour to the entire spectrum/all colours). In addition to containing all visible colours, the white light contains invisible infrared light.
The challenge for Ole Bang and his research team is to get the laser to deliver infrared light with the right wavelengths.
“The shorter the wavelength of the infrared light, the more it disperses when we transmit it into the skin. To penetrate deeper into the skin, we therefore need infrared light with a longer wavelength. The OCT system being tested at Bispebjerg Hospital is based on infrared light with a wavelength of 1.3 micrometres. We’re working on raising this to 4 micrometres,” he says.
Although the research team has succeeded in creating infrared light with the widest wavelength spectrum ever, ranging from 1.3 to 13.3 micrometres (μm), the whole spectrum cannot be used for human tissue because the light is absorbed by fluid in the tissue. However, it can be used for solid and non-aqueous materials such as teeth, pills, solar cells, and plastic.
To create this broad wavelength spectrum, the researchers have developed their own special optical crystal fibres, made in a drawing tower at DTU Fotonik.
Tests on patients in 2018
Bispebjerg Hospital expects to get permission to use the improved OCT technology on patients during 2018. To date, the equipment has only been tested on healthy test subjects.
“The new OCT device not only delivers better pictures. It also allows us to scan patients in just a few seconds, instead of the 30-60 seconds we need using conventional OCT equipment. This is really useful when examining say an eyelid, because the tissue must be kept completely still during the scan,” says Mette Mogensen.
The consultant estimates that using the improved OCT technology, up to 60 per cent of diagnoses can be made based solely on the images. For the remaining 40 percent, it will still be necessary to take a tissue sample.
“The great majority of our skin cancer patients will benefit from the faster new imaging, because their diagnosis will be made quickly following a painless examination, with the results available on the same day,” says Mette Mogensen.
Mid-infrared light is invisible to the human eye, but can be used for OCT (Optical Coherence Tomography) imaging.
The wavelength of the infrared light determines what the light can be used for, as absorption of the light by the materials varies for the different wavelengths.
Under the ShapeOCT project, OCT systems are being developed that use infrared light with the following wavelengths:
• 1.3-2 μm: Can penetrate a few millimetres into the skin. Suitable for diagnosing skin cancers.
• 4-7 μm: Can ‘shine’ through hard materials, such as ceramics and plastics. Can be used to detect irregularities in products such as aluminium coffee capsules, pills, and credit cards.
• 3-12 μm: These mid-infrared light wavelengths are also known as the molecular fingerprint band. It is possible to identify specific molecules using these wavelengths. Undesirable substances can be detected, such as pollution in air, soil, and food.