Sleep is the brain’s way of spring cleaning—and effectively removing toxins. During deep sleep, the body is normally completely at rest and unreactive to the brain’s signals. However, this is not always the case. Some people experience such powerful movements during sleep that they are in danger of breaking their arms and legs
These patients are typically referred to the Danish Centre for Sleep Medicine. Here, they spend the night with electrodes attached to different parts of the head and body while connected to a device that can monitor the electrophysiological signals.
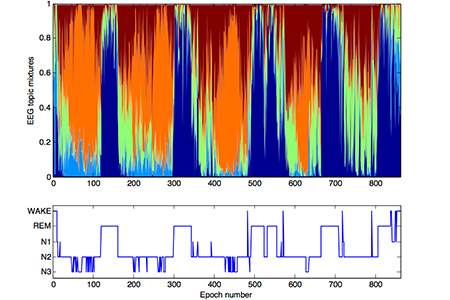
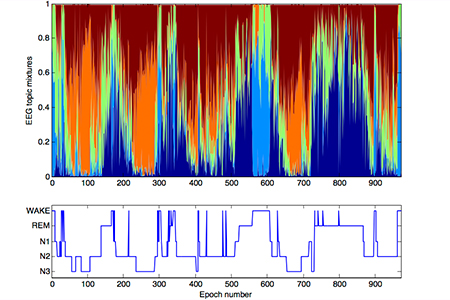
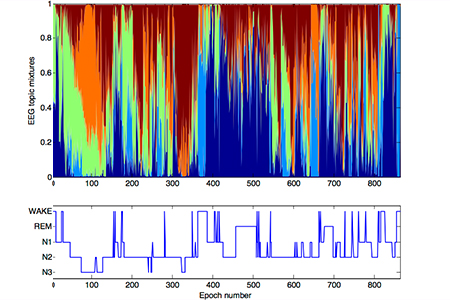
By morning, researchers have a graphical image of sleep, with the different sleep stages represented by colours. The images can, for example, look like the figures on the opposite page for a healthy person, a patient with abnormal movement during dream sleep (IRBD), and a patient with Parkinson’s disease, respectively.
Human consciousness is divided into five stages—wakefulness, REM (dream sleep), non-REM (N) 1, 2, or 3. The five stages are shown in the graphical representation under the colour images, which are the result of the manual evaluation method currently used by doctors who—at 30-second intervals—decide which of the five stages is applicable to the patient. As you can see, in a healthy person’s sleep pattern there is a strong correlation between the dark blue colour and the periods with manually registered REM sleep—just as the orange colour corresponds to N3, and the green to N2.
|
(a) Control subject
By registering the brain’s electrophysiological signals in the course of a night, researchers can gain an overview of a person’s sleep patterns.
The graphs indicate the subject’s various sleep stages. Here, the colour distributions show a regular distribution of REM sleep (dark blue) a non-REM 3 (orange), non-REM 2 (green) and wakefulness (light blue)..
|
|
 |
(b) iRBD patient
This person is suffering from irregular movements during REM sleep (idiopatic rapid eye movement sleep behaviour disorder) as reflected in the colour pattern, where the dark blue fields are ‘disrupted’ by other colours.
|
|
 |
(c) Parkinson patient
In a person whose brain stem is in the process of degradation due to Parkinson’s disease, the mixing of colours is even clearer. The clear delineation between wakefulness (light blue) and REM sleep (dark blue) is erased.
|
|
Data-driven modelling of sleep EEG and EOG reveals characteristiscs indicative of pre Parkinson's and Parkinson's disease by Christensen Jae, Zoetmulder M, Koch H, Frandsen R, Arvaston L, Christensen SR, Jennum P, Sorensen HBD. |
The two evaluation methods correspond well—the computer-generated images simply provide a more nuanced picture. One of the obvious advantages of the new method is that it shows that the brain is in several states simultaneously. A healthy person can easily access several states within a 30-second period—and in the healthy person—it is clear that at the beginning of the night, the sleep stage N3 (corresponding to the orange colour) builds up slowly rather than occurring abruptly, as indicated by the traditional method.
However, before doctors can abandon the old evaluation method with its abrupt 30-second intervals, they must, of course, provide solid evidence to support the use of colour images as a valid tool for diagnosing Parkinson’s disease. And it is precisely this task that postdoc Julie Anja Engelhard Christensen is engaged in.
She started as an MSc student on DTU’s Medicine and Technology study programme and became so captivated by the work with brain signals that she took a PhD with Associate Professor Helge Sørensen from DTU Electrical Engineering and Consultant Poul Jennum from Rigshospitalet Glostrup—along with two researchers from the pharmaceutical company H. Lundbeck A/S—as supervisors. She now holds a full-time postdoc position at the Sleep Centre at Rigshospitalet Glostrup.
"At the Danish Centre for Sleep Medicine, we have a total of seven engineers with a high degree of expertise in signal processing, which is quite unique."
Julie Christensen, postdoc, Rigshospitalet Glostrup.
“The most cited model for sleep regulation is that we have two on/off buttons: you are either awake, or asleep—and sleep can be REM or non-REM. In principle, wakefulness and REM can never occur at the same time, as there is normally a 90-minute interval between sleep and REM,” says Julie Christensen.
“In REM sleep, you are normally paralyzed from the brainstem down, rendering you immobile—REM sleep is the time when the brain is completely free to clean up and rid itself of toxins, and the body should normally not respond physically to dreams. However, the mechanism is defective in people suffering from IRBD, and this defect can be an early marker for Parkinson’s disease.”
“We therefore examine a host of these colour plots to find a marker which can diagnose the IRBD patients—e.g. a weakening of orange dominance or two colours occurring simultaneously. While we have also succeeded in identifying a high risk group, a normal group, and people suffering from a different condition than Parkinson’s disease, we have not yet found an unequivocally clear pattern—partly because the control group is not completely homogeneous. And to be absolutely sure we must, of course, monitor the patients over an extended period of time.”
The ultimate goal is for automatic sleep pattern detection to gradually provide doctors with a precise picture of which parts of the brain that have been destroyed, thus enabling the pharmaceutical industry to work towards developing a medicine that can inhibit degradation—or, at best, stop it.
International collaboration
The sleep centre at Glostrup examines about six patients a day, and similar studies are ongoing at several other locations in Denmark. However, in relation to the global population, data are somewhat scarce so it is very important for the researchers to cooperate with similar centres in Europe and the USA.
Helge Sørensen and Poul Jennum thus maintain a permanent research collaboration with Stanford University, where the first and biggest sleep centre in the world is located. And every year, several of their PhD and MSc students are stationed in Denmark.
Julie Christensen, who has also spent part of her studies at Stanford, elaborates:
“At the Danish Centre for Sleep Medicine, we have a total of seven engineers with a high degree of expertise in signal processing, which is quite unique. At the Californian sleep centre, they have, of course, far more data, which we can draw on. But together with DTU Electrical Engineering, we also cover a gap area for them, as they lack medical engineers for precisely the form of signal processing that we are engaged in here. In the USA, the standards are a little different than our own, but that’s a good thing because hopefully we should be able to arrive at the same clear-cut diagnosis whether you are being examined in Denmark or California.”